The term autoimmune diseases covers a range of disorders that have as a common characteristic the loss of immune tolerance toward one's own tissues. Type 1 diabetes, multiple sclerosis, lupus and primary Sjögren syndrome are all examples of autoimmune diseases.
The epithelial tissues of the skin, mucosae and glands are frequent sites of autoimmune disorders.
Indeed, the most-frequently affected tissues in primary Sjögren syndrome (SSp)¹ are the epithelia of the salivary and lacrimal glands. Lymphocytes infiltrate those glands and provoke a reduction respectively in saliva and tear production. That phenomenon, in turn, causes dry mouth and dry eye symptoms. Lymphocytic infiltration in SSp can also affect other organs such as the lungs or kidneys.
Interestingly, the salivary epithelial cells are not a passive target in SSp, but rather active players in the pathophysiology of the disease: they participate in the maintenance and survival of the infiltrating lymphocytes. However, the mechanisms regulating that role are not fully understood.
The UMR1184S Autoimmune Diseases Team (IDMIT CEA-Jacob/INSERM/Paris-Saclay University/Kremlin-Bicêtre Hospital) teamed with colleagues from the Rheumatology Department of the Kremlin-Bicêtre Hospital to study interactions between salivary epithelial cells (SECs) and T lymphocytes (TLs). In their work, published in Arthritis & Rheumatology, they focused more specifically on the interleukin-7 (IL-7)/interferon (IFN) axis. IL-7 is an important cytokine in the maintenance of TL homeostasis. Earlier studies have shown that IL-7 levels are increased in the salivary glands of patients with SSp.
In their recent study, the UMR1184S-Bicêtre team demonstrated an increase in serum² IL-7 levels in patients with SSp, in comparison to healthy controls. That increase in serum IL-7 was also associated with markers of B lymphocyte activation and signs of SSp activity, such as lymphopenia.
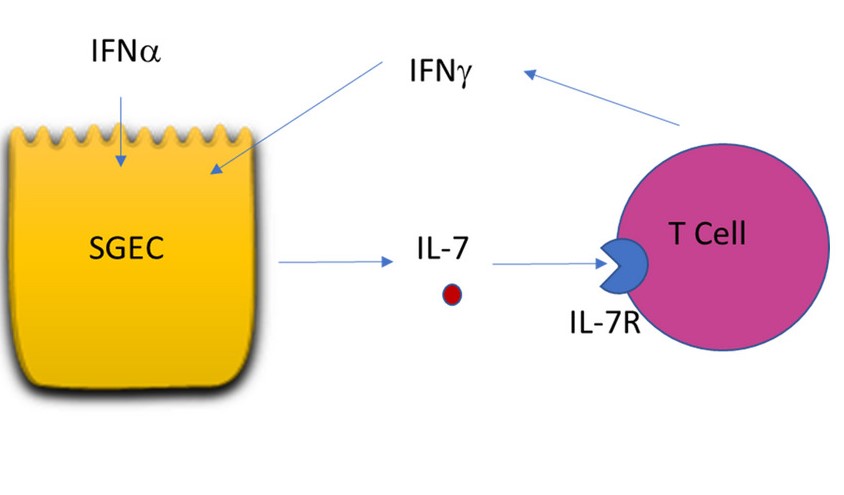
Furthermore, the researchers showed that SECs cultivated from salivary gland biopsies and immunostimulated with poly(I:C)³, IFNα⁴, or IFNγ secreted IL-7. When stimulated by IL-7, TLs from patients with SSp showed greater activation and secretion of IFNγ than did the same cells taken from controls.
The team also performed SSp salivary gland biopsy explantations in the presence or absence of anti-IL-7 receptor (anti-IL-7R) antibodies. The transcriptomics analysis (RNA quantification) of the biopsies and their escaped cells showed that anti-IL-7R antibodies enabled a reduction in IFN-stimulated gene expression.
Considered together, the team's results suggest an IL-7/IFN amplification loop involving SECs and TLs in the setting of SSp. The IFN signature (indicating excessive stimulation of signaling pathways for IFN-induced gene expression) in SSp could explain the increase in IL-7, notably via the local production of it. That local IL-7 production could in turn contribute to TL activation and particularly to IFNγ production in the salivary glands. This UMR1184S-Bicêtre work also opens perspectives with the development of a novel salivary gland tissue culturing model that enabled the demonstration of a tissular reduction in the IFN signature via the use of anti-IL-7R antibodies. Thus, impeding the IL-7/IL-7R axis in the salivary glands of patients with SSp may represent an interesting therapeutic possibility.
1 : Primary Sjögren syndrome mostly affects women and usually around the age of 50 years. Its estimated prevalence ranges from 0.01 to 0.09%.
2 : Serum is what remains of blood once the red and white cells and clotting factors have been removed. Certain molecules are best assayed in serum.
3 : Polyinosinic:polycytidylic acid, abbreviated poly(I:C), is used to simulate a viral infection and thus provoke an immune response.
4 : Interferons (IFNs) are a type of cytokine produced in response to a viral infection (RNA or DNA viruses). There are three types: Type I interferons group most importantly the leukocytic IFN-α and fibroblastic IFN-β; Type II interferons comprise only one member, IFN-γ, produced primarily by natural killer cells and natural killer T cells; Type III interferons are the four IFN-λ, which modulate the immune system in a more muted manner. Each type has its own receptor and signal transduction pathway. Interferons stimulate or inhibit as many as 300 different genes coding for various proteins involved in antiviral defense, inflammation, adaptive immunity, etc. Interferon properties are used therapeutically to treat certain viral infections.